Patient Resources
Patients: What to Expect with your heart surgery
Discover Kai
Experience Kai Today More than just a chatbot, Kai is a smart and friendly companion that can help you with your healthcare needs. Whether you are a patient, a clinician, or a researcher, Kai offers a personalized and convenient way to interact with healthcare information and services. Try Kai today and see how it can make a difference for you.
How Do Our Hearts Work?
The heart is a pump and its function is to circulate blood and nutrients. It is about the size of fists clenched together and weighs approximately 1 ½ pounds. The heart is located in the chest between two lungs and behind the sternum or breastbone. The ribs and sternum protect your heart.

Dr. Khalpey’s Pre-Surgery Cardiac Diet: A Two-Week Plan
This two-week anti-inflammatory cardiac diet is designed to provide diverse and balanced meals for cardiac surgery patients, incorporating key principles of the Mediterranean diet while focusing on anti-inflammatory ingredients.
Prior to Surgery
- 1.
Review your medications, including vitamins and herbal supplements, with your health care providers. Some medications/supplements may need to be stopped before surgery.
- 2.
Elimiate your alchohol intake and stop smoking for at least 2 weeks before surgery.
- 3.
Do not use a razor on your chest or legs within 24 hours of surgery.
- 4.
Attend your pre-procedural screening appointment.
- 5.
Surgical bath should be done 3 times prior to surgery. (Two times the day before surgery, in the morning and at night, then the morning of surgery).
Day Before Surgery
- 1.
Use the anti-bacterial scrub provided to wash your entire body from the neck down, avoiding the genitals, the evening before surgery.
- 2.
You may not eat or drink after 10p.m.(except for approved medication).
Day of Surgery
- 1.
Use the anti-bacterial scrub to wash your entire body from the neck down, avoiding the genitals, again the morning of surgery. Do not apply any lotions, creams, deoderant, or ointments after bathing.
- 2.
Take only the medications you have been instructed to take with a small sip of water.
- 3.
Report to the Surgery/Endoscopy Admitting Area at your instructed time.
Expectations of our Open Heart Patients
Our team strives to facilitate a healing environment that ensures patients undergoing Open Heart Surgery understand their roles in the recovery process. In order to promote the best possible outcomes, your healthcare team has several expectations both during & after your hospital stay.
During your hospital stay you are expected to participate in the following activities:
- 1.
Up to chair for all meals.
- a.
All patients should be sitting up in the chair for each meal.
- 2.
Shower daily. All patients must shower daily ONCE ALL TUBES ARE REMOVED.
- a.
To reduce the risk of infections, patients are asked to please shower and cleanse all incisions daily.
- b.
All dressings should be removed prior to showering unless otherwise indicated by staff.
- c.
The only exceptions to this expectation are the following: I. You are connected to an external pacemaker.
- II.
Respiratory issues.
- III.
You have developed a fast, irregular heart rhythm that prevents you from being taken off of intravenous medications.
- 3.
Walking & Stretching
- a.
All patients must walk 4 times a day at minimum.
- b.
Pictures of various stretching exercises can be found under your Home Activity tab in your surgical heart binder.
- 4.
TED Hose (white stockings worn to compress the lower extremities).
- a.
All patients should be sitting up in the chair for each meal.
- 5.
Dressing changes
- a.
Must be completed daily on all incisional sites and/or puncture sites by nursing staff.
- b.
Incisions should not be covered with a dressing during your shower.
- 6.
Incentive Spirometer
- a.
To be used 10 times an hour while awake to allow deep breathing and help prevent any lung related issues.
If you have any further questions please feel free to contact your Inpatient Care Cardiac Rehab Nurse Educators at either Scottsdale Healthcare location:
***Please bring your surgical heart binder with you on the day of your surgery!***
During the Operation
Robotic Heart Surgery:
Robot-assisted surgeries are used for a number of different heart-related procedures, including repair or replacement of stiff or leaky heart valves, coronary artery bypass grafting (CABG), heart defect repair such as atrial septal defect (ASD) repair or atrioventricular repair (AVSD), tumor removal, to correct atrial fibrillation, a common type of arrhythmia, patent foramen ovale (PFO) closure, and to treat congenital heart conditions. Your surgeon may have other reasons to recommend robot-assisted surgery which will be discussed with you.
Robot-assisted cardiac surgery is heart surgery performed through very small cuts in the chest. With tiny instruments and robot controlled tools, your surgeon is able to perform heart surgery in a way that involves less risk than open-heart surgery as the surgeon does not have to cut through the breastbone to open your chest. Smaller incisions mean that you can heal faster, have decreased chest trauma, have a lower risk of infection, less postoperative pain, and return to activities more quickly. Most people can resume their normal activities after a few weeks.
In some rare cases, your surgeon may not be able to complete the surgery with the use of the robot. In this case, you would need open-heart surgery.
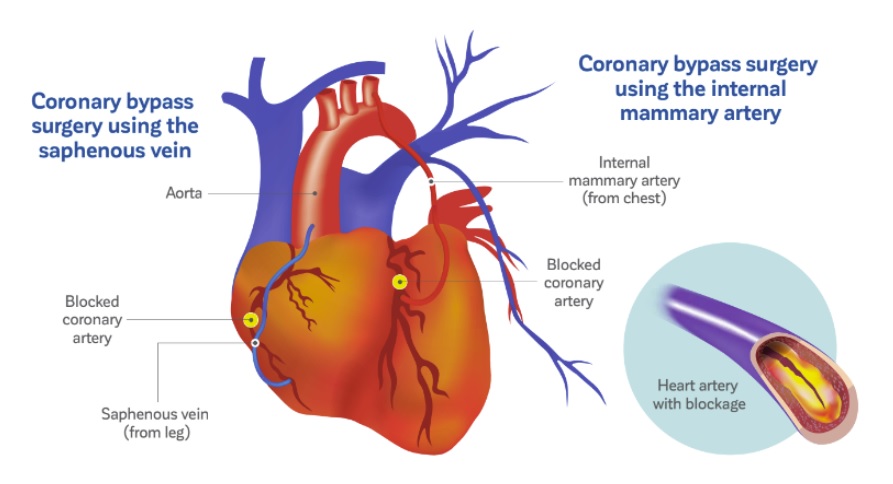
Coronary Artery Bypass Surgery:
If one or more of your coronary arteries (the vessels that carry blood to your heart muscle) are blocked, blood cannot flow to the heart muscle. In this case, the heart muscle may die (heart attack). Coronary artery bypass surgery creates a path for blood to flow around a blockage and helps prevent a heart attack. First, a healthy blood vessel (graft) is taken from another part of the body. Taking this graft usually does not affect blood flow in that body part. These arteries or veins are then surgically connected to the coronary arteries on the surface of the heart to create a way for blood to flow around the blockage. If you have multiple blockages, more than one bypass may be done. A common abbreviation for this type of surgery is CABG, which stands for Coronary Artery Bypass Grafting.
Coronary artery bypass surgery can be done with the heart still (on pump) or with the heart beating (off pump). In the on-pump procedure, a heart-lung machine does the work of your heart and lungs during surgery. The machine supplies the blood with oxygen and pumps it back through the body. Your own heart and lungs start working again after the bypass is completed.
Heart Valve Surgery
Repair of the Valve:
Whenever they can, surgeons prefer to repair a valve rather than replace it. The most common kind of repair involves sewing a ring around the entrance to a valve to improve its size or shape. Another involves cutting tissue to let leaflets open or close better.
Replacement with a Mechanical Valve:
Mechanical valves are made of metal or hard carbon. Mechanical valves can last for decades, but blood tends to stick to them, forming clots. If you receive a mechanical valve, you will need to take Warfarin, an anticoagulant medication, for life to prevent blood clots.
Replacement with a Tissue Valve:
A tissue valve usually comes from a pig or cow. Blood does not clot as easily on tissue valves, so patients may need Warfarin for only a short period of time. Tissue valves may wear out faster than mechanical valves, so they may have to be replaced sooner.
Left Atrial Appendage Ligation:
This procedure is for surgical patients with and without atrial fibrillation. For patients with atrial fibrillation or history of atrial fibrillation, the most serious risk is having a stroke. Blood can pool and form clots in your left atrial appendage (LAA). If a blood clot breaks loose it may travel through your blood vessels and eventually cause an obstruction in your brain causing a stroke. Surgical patients who do not have atrial fibrillation are at an increased risk for developing atrial fibrillation post-operatively. Your left atrial appendage (LAA) is a small, ear-shaped sac in the muscle wall of the left atrium (top chamber of the heart). It is unclear what function, if any, the left atrial appendage (LAA) performs. Whether you have atrial fibrillation, history of atrial fibrillation, or are surgical patient with the risk of developing post-operative atrial fibrillation your most serious risk is having a stroke.
Impella
The Impella is a device that can support the body by doing some of the work of the heart when it is failing or needs to rest for recovery. It can be used for a short period of time in the OR or cath lab, or it can be left in for several days and the patient cared for in the ICU if needed. The Impella is a very small heart pump that is usually inserted into the left side of the heart and pulls blood from inside the heart and pushes it out into the aorta, the major blood vessel of the body. This helps take some of the workload off of the heart so it can heal and helps provide oxygenated blood to the body when the heart can’t. The Impella can also be placed in the right side of the heart to push blood into the lungs if the right side of the heart is failing. Your care will be similar for either type of heart support.
After Surgery
- 1.
Follow up appointment with cardiologist.
- 2.
Follow up appointment with cardiac surgeon.
- 3.
Outpatient Cardiac Rahab appointment
- 4.
Primary care provider to be seen within 2-4 weeks. Please call to setup follow up visit.
Minimally Invasive Valve Surgery
The following information highlights activity after discharge: Remember you did NOT have a sternotomy, therefore you do not have any restrictions in terms of arm movement. There is no restriction on your range of motion. You can raise your arms over your shoulders and use your arms to help you in and out of a chair and/or bed. Your only restriction is pain. If you do a movement that is painful, please stop.
Shower:
- Leave the shower door open about 6 inches and bathroom door open to reduce steam buildup.
- Use lukewarm water over the incisions.
- Use soap on your hand and gently pat the incisions. Rinse with water. Pat it dry.
- Shower daily until the incisions are healed and the scab has fallen off.
- Do not remove the scab. Leave it alone. Healing may take approximately 6 weeks.
- Do not apply lotions, powders, ointments, bandages or anything else on your incisions. Leave your incision dry and open to air. If you have drainage from any incision site, please call your surgeon.
- Do not take a tub bath, sit in a hot tub or Jacuzzi, or swim for at least 6 weeks or until your doctor says it is OK. (Do not submerge your incision)
- Protect your incisions from over exposure to sunlight, as they will sunburn more easily the first year.
Legs:
- Avoid crossing your legs because this impairs circulation.
- Avoid sitting in one position or standing for a prolonged period of time.
- Elevate your leg on a stool or coffee table when sitting. You can lie on a couch and elevate your legs on the arm of the couch.
- If you continue to have leg swelling or it becomes worse, notify your cardiologist.
- If TED hose are prescribed, wear them for at least two weeks after discharge. These are to be put on in the morning and removed in the evening.
Driving:
- Avoid driving until your follow-up appointment with the surgeon. Your surgeon must clear you to drive.
- Wear your seat belt while riding in the vehicle.
- Your surgeon may want you to be able to walk a total of 20 minutes at one time before releasing you to drive again.
Stairs:
- Unless your doctor tells you differently, you can climb stairs. Take them at a slow pace. Stop and rest if you tire.
Sexual Activity:
- You can resume sexual relations when you feel comfortable. For many people, this is about 2 to 4 weeks after discharge, unless instructed differently by your doctor.
Work:
- Check with your surgeon before returning to work. Depending on your job, you may feel like returning to light work 3 to 4 weeks after surgery.
Exercise Basics:
- You need a balance of rest and exercise while you recover. Plan to rest between activities and take a short nap as necessary. Resting also includes sitting quietly for 20 to 30 minutes. Rest 30 minutes after meals before you exercise.
- Walking is one of the best forms of exercise because it increases circulation throughout the body and to the heart muscle. It is important to increase your activity gradually. Walk at your own pace. Stop and rest if you are tired. Try to walk 10-minute intervals to begin with and increase the length of time to 20 minutes as you tolerate.
- Pace activities throughout the day. Try not to do too many things at one time.
- Begin using the Home Activity Progress Record.
- Before you walk, the stretching exercises can be done 1 – 2 times per day preferably.
- Do not hold your breath during activity.
- One stretching activity recommended post-operatively is to walk your arm gradually up the wall as tolerated on surgical side 2-3 times daily until full range of motion is restored.
Procedure Video

Frequently Asked Questions
What do I need to know about heart or lung surgery?
Every patient and procedure is unique in their own way, but we’ve put together a resource page for you on What to Expect while you are a patient at Phoenix Cardiac Surgery.
What is a Heart Attack?
The medical term for a heart attack is a myocardial infarction. All muscles in the human body require oxygen to function. A heart attack/myocardial infarction occurs when the heart muscle does not get enough oxygen, resulting in damage to the muscle of the heart.
The coronary arteries are responsible for the delivery of oxygen to the heart muscle. When these arteries become severely blocked or narrowed, they restrict the flow of oxygen to the heart. The result may be a heart attack.
What are the symptoms of a Heart Attack?
The symptoms of a heart attack vary, but here are the most common:
- Squeezing, burning, tightness, fullness, or pressure across the chest, which may radiate to the shoulder, arms (especially the left), neck, jaw, teeth, earlobes, as well as the upper back between the shoulder blades.
- Numbness or tingling in the arms or hands.
- Nausea and vomiting
- Sweating
- Palpitations
- Dizziness
- Loss of consciousness
Note: You can suffer a heart attack with any or all of these symptoms. If you think you may be experiencing a heart attack, dial 911 immediately.
Can changing my diet reduce risk of a Heart Attack?
Yes! Your diet does impact your risk of heart disease. Modifying your diet to control weight, blood sugar, and cholesterol levels can help you avoid a heart attack, as well as improve your overall health.
Can exercise help prevent heart disease?
Exercise has long been recognized as a way to combat certain coronary risk factors, and it’s a critical part of successful recovery from open heart surgery.
Instructions for exercise will typically be provided by physical therapy, nursing, and inpatient cardiac rehab personnel. Knowing how to gauge your exertion level and take your pulse is helpful for everyone, regardless of your heart health.
Will I need a blood transfusion?
Physicians at Phoenix and Yavapai Cardiac Surgery perform over 90% of routine cardiac operations without giving a single unit of blood. We are key opinion leaders around the world on Patient Blood Management. We use a multi-specialty, multi-modality approach to heart surgery so that surgery is performed without having to rely on blood transfusions, leading to the best possible outcomes.
Patient Blood Management (PBM) is the scientific use of safe and effective medical and surgical techniques designed to conserve a patient’s own blood and decrease bleeding in an effort to improve patient outcome. This technique is design to minimize or avoid the need for the transfusion of donor blood components. Many people refuse blood transfusion of some or all blood products. This could be due to their religious believes (e.g. Jehovah’s witness) while others do so as a result of healthcare concerns or other personal convictions.
In the US, many cardiac surgical programs still use blood transfusions in over 60% of patients undergoing heart surgery even while hundreds of studies have now shown that patients who get even one unit of blood or blood products (fresh frozen plasma, platelets, etc.) have a higher complication rate and mortality. These risks can range from infections to allergic reactions that can be life threatening. There is also evidence that by avoiding blood transfusions, patients will have faster recoveries and shorter hospital stays.
Learn more about Patient Blood Management from the The Society for the Advancement of Patient Blood Management (SABM.org).
What are the warning signs of heart problems after surgery?
You should call your doctor immediately if you notice any of the following:
- Weight Gain: You gain more than 3 pounds in one day or 5 pounds in one week. Weigh yourself every day and track your weight.
- Chills or Fever: You have chills, sweating, or a fever over 100.4 degrees for more than a day.
- Irregular Heartbeat: Your heart seems to be beating fast or slow, or skipping beats.
- Trouble Breathing: You have shortness of breath while resting.
- Chest or Shoulder Pain: You have pain or tightness in your chest or shoulder that worsens with deep breathing or coughing.
- Swelling around Incision: You have swelling, redness, oozing, or tenderness around your chest incision.
- Bleeding: You have unexplained bruising or bleeding.
Heater-cooler devices and NTM infections
On October 13, 2016, the Centers for Disease Control (CDC) issued a Health Alert Notice to patients and hospitals regarding the risk of NTM infections from Stöckert heater-cooler devices used during open-heart surgery. While risk of infection is low, it is important to consult with your doctor.
Patients who have had open-heart surgery and are having the following symptoms should seek medical care:
- night sweats
- muscle aches
- weight loss
- fatigue
- unexplained fever
As recommended by the CDC, we are working to alert anyone who underwent a surgical procedure with cardiopulmonary bypass (CPB), including cardiac surgery, general thoracic surgery, or vascular surgery from June 2011 to August 2016.
As advised by the CDC, we no longer use the Sorin Stöckert 3T heater-cooler devices.
Read more from the CDC here.