A Framework for the Development of Artificial Intelligence as a Co-Pilot in the Cardiac Operating Room
The cardiothoracic operating room (OR) is a critical environment that involves many dynamics which impact the healthcare delivery process on multiple levels including clinical outcomes, costs, and patient safety. Within the operating room is a massive amount of continuous inflow of data for the surgeon to assess, such as multiple arterial lines, ECG waveforms, oxygenation and cerebral perfusion waveforms and TEE’s, not to mention the pre operative labs and imaging found within the EMR. With the integration and use of digital tools and algorithms within the cardiac OR space, validated predictive models are being used for treatment planning and procedures, which has been shown to reduce mortality rates and adverse outcomes for procedures like CABG operations. Among the adoption of digitization in the OR, the use of Artificial intelligence (AI) and machine learning (ML) have the most potential to make a significant impact, as these new technologies have the clinical utility to truly augment surgeon decision making and treatment planning in real-time. By harnessing the massive amount of data available in the OR via multi-modality technologies and compiling them into useful algorithms, the surgeon will be able to make informed real-time decisions to better improve individual patient outcomes and avoid potential complications.
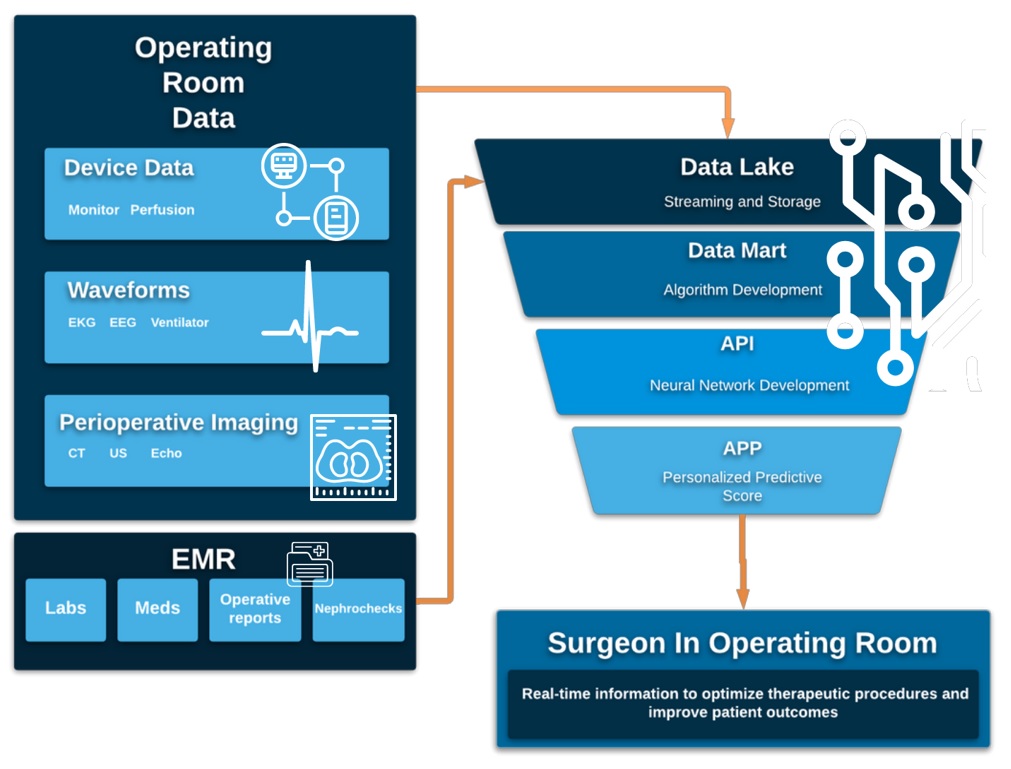
The creation of an AI ecosystem in the OR space requires integrating information from multiple devices including non-invasive equipment such as waveform monitors and ultrasound imaging that can continuously monitor patient values and using machine learning compile that information with EMR imaging and labs to create an accurate predictive model to inform surgical decision-making. A recent study which used AI deep learning models to assess preoperative imaging to predict surgical complexity and outcomes of abdominal wall reconstruction showed that the AI was more accurate than a panel of expert surgeons and furthermore was able to accurately predict surgical site infection (Elhage et al 2021). While several variables that can be added to the AI algorithms have been studied, no one has yet undertaken the massive effort to build an AI ecosystem in the OR which is capable of seamlessly integrating all of the information and variables continuously streaming, often unseen, past the surgeon’s consciousness as they focus on operating. With this continuous monitoring being fed into AI with machine learning, integrated with EMR information, surgeons can make real-time critical clinical decisions informed by instantaneous data, which can ultimately improve the clinical status and outcomes of their patients.
Prediction of Graft Patency in Coronary Artery Bypass Grafting
Coronary artery disease (CAD) is the most common cause of heart disease, and the management of cardiac disease places a significant burden on the healthcare system. While the CABG procedure is the treatment gold standard, it is reported that up to 15% of Saphenous Vein grafts (SVGs) occlude within a year of a CABG, and within 10 years about 50% of patients develop SVG failure. Technical error and graft spasm have been identified as reasons for thrombosis and early SVG failure (Goldman et al, 2004, and Bourassa et al, 1982). These identified shortcomings and risks to the success of the CABG operation can be preemptively identified with a developed dynamic AI algorithm using multiple clinical values, including pulsatility flow index and transit-time flow measurement.
Pulsatility flow index (PI) is a critical measure that can be used as a predictor and marker in cardiac surgery, as well as being used as a measure to evaluate a bypass graft flow14,35. The clinical utility of PI is to evaluate and estimate peripheral vascular resistance using flow resistance (Aleksic, et al., 2004) and it has also been validated in other studies to be a marker for post-surgical success (Rong et al., 2019). Along with PI values, transit-time flow measurement (TTFM) is a validated clinical value, and is the gold standard for intraoperative detection of graft failure . The TTFM is directly proportional to the blood flow, and is a considered a quality control tool for graft evaluation, however, there is limited literature in the use TTFM for predicting long term outcomes and performance6. AI algorithms can incorporate the noninvasive PI index along with TTFM, ultrasound, flowmeters and other more invasive techniques for improved evaluation of graft success and to accurately predict patient outcomes for pre and post-surgical interventions, 4,8,25
Prediction of Acute Kidney Injury: NIRS Monitoring and Oxygen Delivery
During cardiac surgery, oxygen delivery while on bypass, is a critical determinant of perfusion, and affects organ function.22,7,13. Acute kidney injury (AKI) is a severe complication of cardiac surgery, and is correlated with a significant increase in risk for developing infection complications, which increases mortality rates, length of hospital stay, and healthcare costs17.
In cardiac surgery, near infrared spectroscopy (NIRS) monitoring is commonly used to measure cerebral oxygenation (rSO2), however, NIRS can also monitor oxygen circulation (DO2) for the kidneys. NIRS as a diagnostic, monitoring tool at the bedside can predict complications, especially AKI, and be used in postoperative treatment and care planning21,24. NIRS has only been studied as a single value in clinical management, but its ability to monitor kidney function during cardiac bypass surgery provides another real-time clinical data element to be another stackable value as a part of the predictive algorithm and its information can help change current management (Nenna, et al. 2017). This AI driven system shows promise, as a study was done in 2019 which utilized Google’s DeepMind AI to predict AKI in critically ill patients with a lead time of 48 hours compared to current clinical practice (Tomašev et al 2019). This advanced predictive algorithm buys doctors valuable time to prevent and treat AKI sooner, preventing more serious sequelae34.
Prediction of Cerebrovascular Accident and Neuroinflammation
AI can also be utilized to predict which patients are at risk for Post Pump Syndrome (PPS). PPS can be defined as ARDS following Cardiopulmonary bypass (CPB). It is believed that the induced ARDS can cause a priming of polymorphonuclear leukocytes (PMN) causing them to sequester in the lung without lung injury (Picone et al., 1999). EEGs can be used to evaluate PPS, as changes can be observed in real-time, allowing the surgeon to make adjustments to their surgical treatment. In a retrospective study on identifying PPS, researchers found that EEGs showed generalized slowing and generalized triphasic patterns, and showed lateralized slowing, focal epileptiform discharges, electrographic seizures (Hanif et al, 2014). These warning signs can be layered into the AI ecosystem algorithms, to help predict and avert this dire complication.
AI Informed Ventilator Management
When using mechanical ventilation, individual patient physiology and response to the disease states must be carefully fine-tuned to prevent complications (Hickey, 2020). Mechanical vents can be set to different breathing techniques and management, and the settings can greatly affect the response of respiratory regulation and ventilation (Beutler et al, 2016). Contemplative practices can control these breathing techniques which can affect the autonomic response, and can alter the respiratory regulation and reduce hypoxic and hypercapnic ventilatory responses (Gerritsen and Band, 2018, Beutler et al, 2016). The principles of these breathing techniques and practices should be integrated in the management strategies for patients that are on bypass to reduce lung damage and inflammation. Recent clinical studies have also concluded that AI computed outcomes in the ICU have accurate results (0.94 and 0.93) (Pirracchio 2015, and Aczon 2019). AI algorithms can be used to optimize every patient’s individual ventilator settings. The improvement in ventilation settings would reduce time on vents and furthermore reduce complications including ARDS.
Ventilator weaning protocols are also key decision points that can affect clinical outcomes, but are also challenged by wide variability practices. This is an issue that AI can step in to solve, as a clinical study found that AI algorithms outperformed clinical practice by comparing re-intubation rates on ventilated patients (Prasad 2019). While AI tools and algorithms have been developed and tested for mechanical ventilators, the use of AI will continue to grow with the management of ventilator settings and adjusting for individual patient symptoms, biomarkers, and progression to reduce the time on ventilation, and side effects.

Conclusion:
Clinical decision making is a sophisticated process that includes the evaluation of multi-modal data points as the patient evolves through the surgical workflow during the course of their surgery and post-operative care. This decision making is subject to many flaws such as clinician-bias, outdated risk calculators and variability between hospitals but furthermore, it is a static process as decisions are made based on previous clinical values that take hours to days to be sampled and processed. Through the use of AI algorithms, surgeons can have their clinical decisions augmented through a dynamic AI ecosystem right there with them in the OR. The live-stream capturing and processing of multiple clinical data points can be harnessed all together to produce a predictive model and algorithm that can assist physicians in making critical real-time decisions to improve clinical outcomes. The OR ecosystem that we have created is built on a cloud platform which enables real-time decision making, with the capturing of changing values, and enhances the ability to make timely decisions. Defining better metrics and evaluating hidden connections which affect patient outcomes can be unmasked by approaching common problems in a novel way with the assistance and further development of clinical augmented intelligence tools.



