Predicting Heart Failure and Sudden Cardiac Death in Atrial Fibrillation Patients Using Artificial Intelligence
Authors: Amina Khalpey, PhD, Jessa Deckwa, BS, Zain Khalpey, MD, PhD Atrial fibrillation remains to be the most clinically significant arrhythmia seen in clinical practice. Prevalence is about 1–3% in the general population but rises with age (up to 9%, aged ≥65 years; up to 17%, ≥80 years), presence of comorbidities and male sex, and varies with ethnicity, region, and screening method used (1). AF is associated with increased risk of morbidity (up to five-fold increase in stroke, and lesser increases in heart failure, and cognitive impairment) and two-fold and 1.5-fold increase in all-cause mortality in women and men, respectively (3,4,5,6). Atrial fibrillation (AF) is a condition in which the heart’s upper chambers (atria) beat in an irregular, rapid, and uncoordinated fashion (2). AF also causes the heart to pump less effectively, leading to congestion in the lungs and other organs. This can eventually lead to heart failure, a condition in which the heart is unable to pump enough blood to meet the body’s needs. While stroke prevention has been the primary focus of therapy for AF, heart failure is the most common cause of death among individuals with atrial fibrillation, and one of the leading causes of hospitalization (10,11,12). Many of the risk factors including hypertension, obesity, ischemic heart disease, rheumatic and valvular heart disease (13) are possible targets for both primary prevention of AF and prevention of its complications, including stroke and heart failure (14). There is also evidence that an increased burden of AF is associated with worsening of heart failure symptoms (15). A screening implementation of AF could lead to earlier diagnosis and further prevent the potential onset of stroke, heart failure, and other cardiac diseases. The screening system will allow for ECG evaluation upon presentation with specific comorbidities to ensure a holistic view of the patient is evaluated. When obtaining an ECG for AF evaluation implementing heart rate variability (HRV) as a metric could be vital in providing insight into onset and pathway of atrial fibrillation. Predicting heart failure in patients with atrial fibrillation is a critical issue in healthcare. The use of an artificial intelligence technology called machine learning on heart rate variability (HRV) and high frequency to low frequency ratios (HF/LF) can help in early diagnosis and prediction of heart failure in these patients. Moreover, the risk of sudden cardiac death (SCD) can also be evaluated using these parameters. Heart rate variability is a non-invasive and cost-effective method of assessing the autonomic nervous system’s activity. HRV is an important marker of cardiac health and can be used to evaluate the risk of heart failure in patients with atrial fibrillation. The high frequency to low frequency ratio (HF/LF) is a commonly used parameter for evaluating HRV and is calculated as the ratio of the high-frequency power to the low-frequency power of the HRV spectrum. Machine learning algorithms, such as decision trees, random forests, and support vector machines, can be used to predict heart failure in patients with atrial fibrillation based on HRV and HF/LF parameters. These algorithms can be trained using a large and diverse dataset of HRV and HF/LF parameters from patients with atrial fibrillation and heart failure. Prospective data of self-recording fingertip PPG intermittently from a standard smartphone shows promise for detecting AF7. However, a 2020 survey of 588 healthcare professionals showed almost 70% believe we are not yet ready for mass consumer-initiated AF screening using wearables/apps (8). This suggests that smartphones/PPGs may allow more effective global screening and diagnosis of AF at some stage in the future (possibly within the next decade), provided that the technology matures adequately, the burden of data analysis and follow-up can be managed, and issues of privacy are adequately anticipated. A potential alternative or addition to using an ECG would be wearables/apps and devices that utilizes modern computing technology to examine existing clinical specimens, samples, or data (including ECG data) to identify patients at high risk of actionable AF, or even cardiovascular disease (9). However, the large-scale Apple (17), Huawei (18), and Fitbit (NCT04380415) Heart Studies have illustrated the potential of fast, nationwide recruitment of screening participants and demonstrated low rates of false positives among participants who completed the screening. The vast majority of participants were younger than 50 years old and drop-out rates were high. The studies also showed that consumer-led AF screening leads to increased use of healthcare resources in the short term. First, arrhythmias require review and verification by a health professional. Secondly, other arrhythmia findings will trigger additional contacts with the healthcare system for verification. Thirdly, consumer-based AF screening will also be conducted by individuals without stroke risk factors. There is a lack of evidence on the implications and the benefits of screening in patients who are not at risk of stroke, and in young populations. Sudden cardiac death (SCD) is a sudden, unexpected death caused by a malfunction in the heart’s electrical system. It is usually caused by an arrhythmia, an abnormal heart rhythm such as atrial fibrillation, which can disrupt the heart’s ability to pump blood. In addition to HRV and HF/LF parameters, the risk of sudden cardiac death (SCD) can also be evaluated using machine learning algorithms. SCD is a major concern in patients with atrial fibrillation, and early prediction can help prevent it. The risk of SCD can be evaluated using various factors, such as the presence of structural heart disease, the presence of heart failure, and the type of atrial fibrillation. Machine learning algorithms can be trained using a large and diverse dataset of these risk factors to predict the risk of SCD in patients with atrial fibrillation. The algorithms can then be used to evaluate the risk of SCD in individual patients and guide appropriate therapeutic interventions. Machine learning algorithms can be an effective tool for predicting heart failure and the risk of sudden cardiac death in patients with atrial fibrillation. The use of HRV and HF/LF parameters and risk factors can provide valuable information for early diagnosis and intervention, which can help prevent heart failure and SCD in these patients. Artificial intelligence has the potential to unravel the complex pathophysiology leading to atrial cardiomyopathy and AF, early AF detection, prognosis, and precision treatment, but its role, circumstances of its application, and the optimal methods need to be defined. 1. Freedman B, et. al. World Heart Federation Roadmap on Atrial Fibrillation – A 2020 Update. Glob Heart. 2021 May 27;16(1):41. doi: 10.5334/gh.1023. PMID: 34211827; PMCID: PMC8162289. 2. Lopes LA, Agrawal DK. Post-Operative Atrial Fibrillation: Current Treatments and Etiologies for a Persistent Surgical Complication. J Surg Res (Houst). 2022;5(1):159-172. doi: 10.26502/jsr.10020209. Epub 2022 Mar 28. PMID: 35445200; PMCID: PMC9017863. 3. Benjamin EJ, Wolf PA, D’Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of Atrial Fibrillation on the Risk of Death. Circulation. 1998; 98(10): 946–52. DOI: 10.1161/01.CIR.98.10.946 4. Stewart S, Hart CL, Hole DJ, McMurray JJV. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am J Med. 2002; 113(5): 359–64. DOI: 10.1016/S0002-9343(02)01236-6 5. Andersson T, Magnuson A, Bryngelsson I-L, Frøbert O, Henriksson KM, Edvardsson N, et al. All-cause mortality in 272 186 patients hospitalized with incident atrial fibrillation 1995–2008: A Swedish nationwide long-term case-control study. Eur Heart J. 2013; 34(14): 1061–7. DOI: 10.1093/eurheartj/ehs469 6. Sepehri Shamloo A, Dagres N, Müssigbrodt A, Stauber A, Kircher S, Richter S, et al. Atrial Fibrillation and Cognitive Impairment: New Insights and Future Directions. Heart Lung Circ. 2020; 29(1): 69–85. DOI: 10.1016/j.hlc.2019.05.185 7. Brasier N, Raichle CJ, Dörr M, Becke A, Nohturfft V, Weber S, et al. Detection of atrial fibrillation with a smartphone camera: first prospective, international, two-centre, clinical validation study (DETECT AF PRO). Europace. 2019; 21(1): 41–7. DOI: 10.1093/europace/euy176 8. Boriani G, Schnabel RB, Healey JS, Lopes RD, Verbiest-van Gurp N, Lobban T, et al. Consumer-led screening for atrial fibrillation using consumer-facing wearables, devices, and apps: A survey of health care professionals by AF-SCREEN international collaboration. Eur J Intern Med; 2020. DOI: 10.1016/j.ejim.2020.09.005 9. Lopez-Jimenez F, Attia Z, Arruda-Olson AM, Carter R, Chareonthaitawee P, Jouni H, et al. Artificial Intelligence in Cardiology: Present and Future. Mayo Clin Proc. 2020; 95(5): 1015–39. DOI: 10.1016/j.mayocp.2020.01.038 10. Healey JS, Oldgren J, Ezekowitz M, Zhu J, Pais P, Wang J, et al. Occurrence of death and stroke in patients in 47 countries 1 year after presenting with atrial fibrillation: a cohort study. Lancet. 2016; 388(10050): 1161–9. DOI: 10.1016/S0140-6736(16)30968-0 11. Schnabel RB, Yin X, Gona P, Larson MG, Beiser AS, McManus DD, et al. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: A cohort study. The Lancet. 2015; 386(9989): 154–62. DOI: 10.1016/S0140-6736(14)61774-8 12. Rahman F, Wang N, Yin X, Ellinor PT, Lubitz SA, LeLorier PA, et al. Atrial flutter: Clinical risk factors and adverse outcomes in the Framingham Heart Study. Heart Rhythm. 2016; 13(1): 233–40. DOI: 10.1016/j.hrthm.2015.07.031 13. Oldgren J, Healey JS, Ezekowitz M, Commerford P, Avezum A, Pais P, et al. Variations in cause and management of atrial fibrillation in a prospective registry of 15,400 emergency department patients in 46 countries: The RE-LY Atrial Fibrillation Registry. Circulation. 2014; 129(15): 1568–76. DOI: 10.1161/CIRCULATIONAHA.113.005451 14. Chung MK, Eckhardt LL, Chen LY, Ahmed HM, Gopinathannair R, Joglar JA, et al. Lifestyle and Risk Factor Modification for Reduction of Atrial Fibrillation: A Scientific Statement From the American Heart Association. Circulation. 2020; 141(16): e750–e72. DOI: 10.1161/CIR.0000000000000748 15. Wong JA, Conen D, Van Gelder IC, McIntyre WF, Crijns HJ, Wang J, et al. Progression of Device-Detected Subclinical Atrial Fibrillation and the Risk of Heart Failure. J Am Coll Cardiol. 2018; 71(23): 2603–11. DOI: 10.1016/j.jacc.2018.03.519 16. Schnabel RB, et al. Early diagnosis and better rhythm management to improve outcomes in patients with atrial fibrillation: the 8th AFNET/EHRA consensus conference. Europace. 2023 Feb 8;25(1):6-27. doi: 10.1093/europace/euac062. PMID: 35894842; PMCID: PMC9907557. 17. Perez MV, Mahaffey KW, Hedlin H, Rumsfeld JS, Garcia A, Ferris T, et al.. Large-scale assessment of a smartwatch to identify atrial fibrillation. N Engl J Med 2019;381:1909–17. 18. Guo Y, Wang H, Zhang H, Liu T, Liang Z, Xia Y, et al.. Mobile photoplethysmographic technology to detect atrial fibrillation. J Am Coll Cardiol 2019;74:2365–75.Introduction
Atrial Fibrillation Is a Common Cause of Heart Failure
Evidence-based implementation of systematic screening for atrial fibrillation (17)

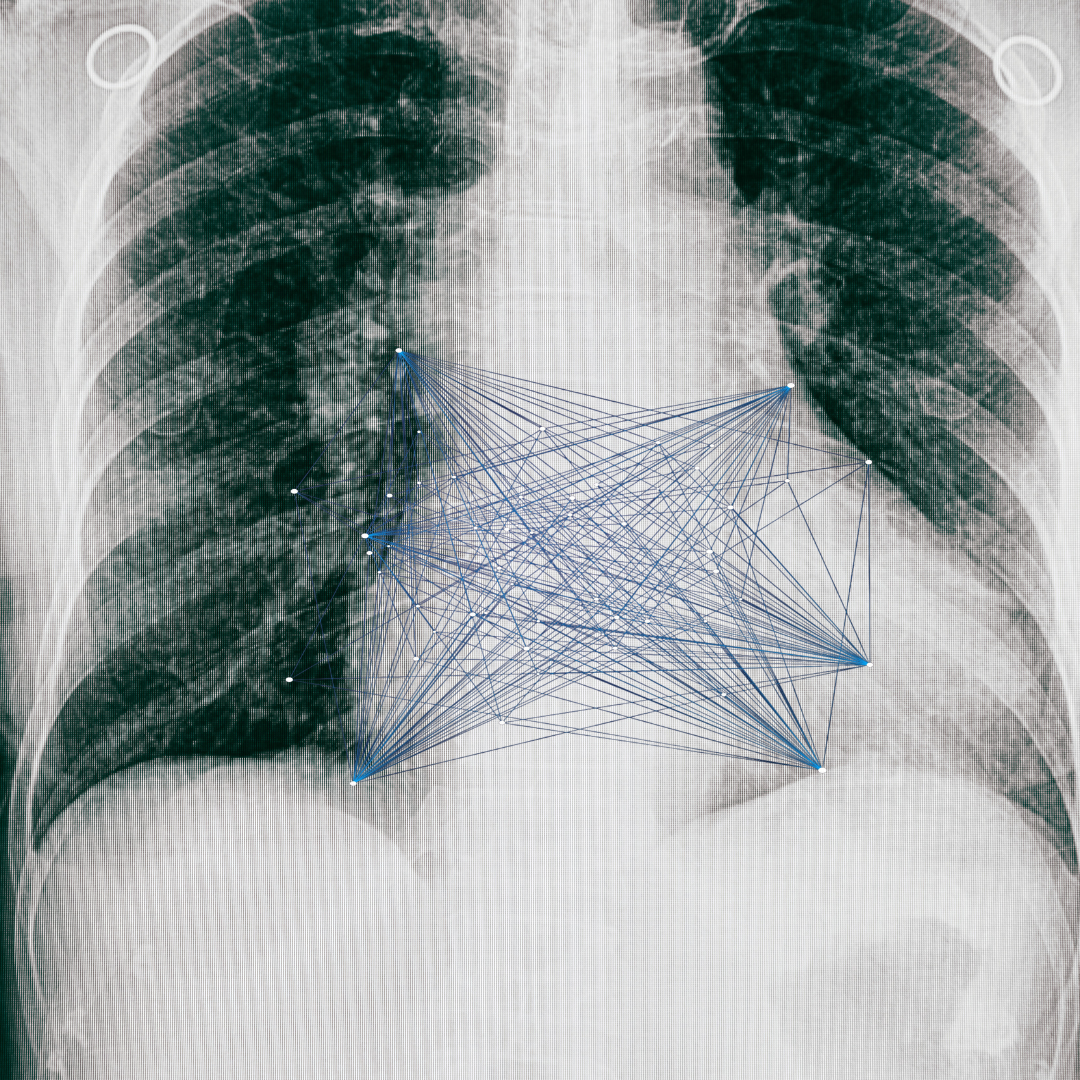
Utilizing Machine Learning to Predict Heart Failure
How Sudden Cardiac Death From Heart Failure Can Be Predicted
Artificial Intelligence Tools like Machine Learning Can Revolutionize Heart Disease
References:



